Introduction
Osteoarthritis ICD 10 is one of the most common joint disorders, affecting millions of people worldwide. It is a degenerative disease that causes the cartilage in joints to wear down over time, leading to pain, stiffness, and decreased mobility. Accurate classification and coding of osteoarthritis are essential for proper documentation, insurance reimbursement, and medical research. In healthcare systems globally, the ICD-10 codes for osteoarthritis provide a standardized way of recording this condition.
This blog explores the basics of osteoarthritis, its symptoms, risk factors, treatment options, and how it is categorized within the ICD-10 system.
What is Osteoarthritis?
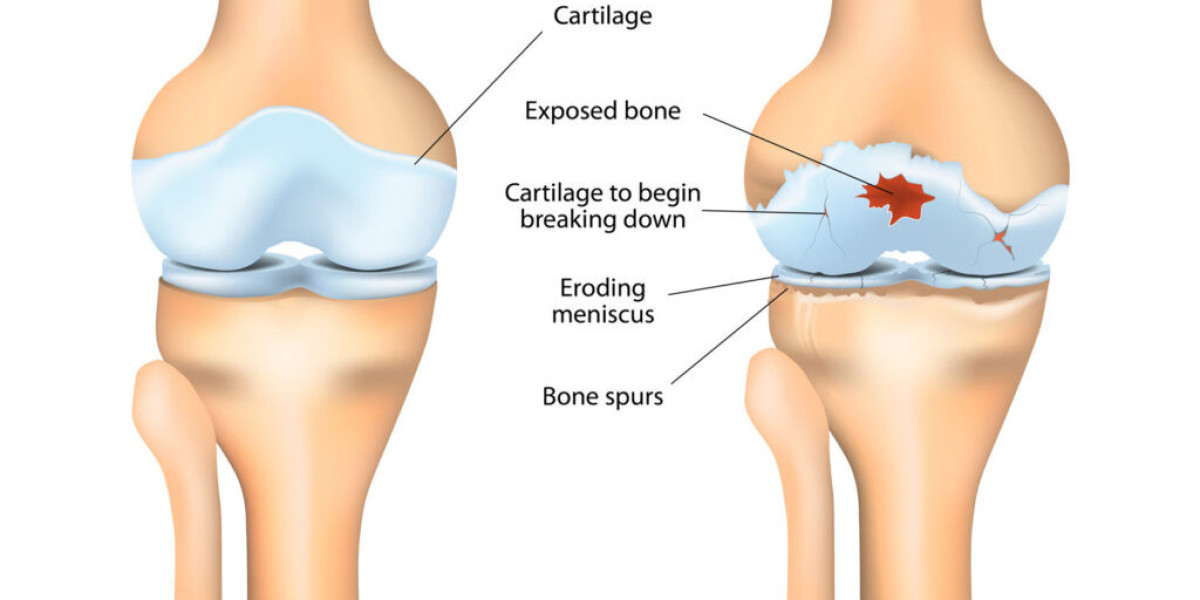
Osteoarthritis ICD 10 is often referred to as “wear-and-tear arthritis” because it develops when the protective cartilage cushioning the ends of bones gradually deteriorates. Over time, this leads to bone-on-bone contact, pain, and limited mobility. Unlike autoimmune types of arthritis (such as rheumatoid arthritis), osteoarthritis is primarily mechanical and degenerative in nature.
Key Features of Osteoarthritis:
Gradual onset of symptoms.
Affects weight-bearing joints such as knees, hips, and spine.
Can also affect hands, especially the base of the thumb.
Progressive, with severity increasing over time.
Symptoms of Osteoarthritis
The symptoms of osteoarthritis vary depending on the joint involved but commonly include:
Joint pain that worsens with activity and improves with rest.
Morning stiffness, usually lasting less than 30 minutes.
Swelling and tenderness around the joint.
Grating or popping sounds during movement.
Reduced range of motion in affected joints.
Development of bony growths (osteophytes) in advanced cases.
Risk Factors for Osteoarthritis
Several risk factors increase the likelihood of developing osteoarthritis:
Age – Risk increases with aging.
Gender – Women are more likely to develop OA, especially after menopause.
Obesity – Extra body weight stresses weight-bearing joints like hips and knees.
Genetics – Family history can predispose individuals to OA.
Injuries – Joint injuries or repetitive overuse can accelerate cartilage breakdown.
Occupation – Jobs involving repetitive movements or heavy lifting increase risk.
ICD-10 Coding for Osteoarthritis
The International Classification of Diseases, 10th Revision (ICD-10) is the coding system used worldwide to classify and record diseases, including osteoarthritis. For healthcare providers and coders, accurate documentation of osteoarthritis using ICD-10 codes is critical for patient records, treatment planning, insurance claims, and research.
Common ICD-10 Codes for Osteoarthritis:
M15 – Polyosteoarthritis
M15.0: Primary generalized osteoarthritis
M15.9: Polyosteoarthritis, unspecified
M16 – Osteoarthritis of the Hip
M16.0: Primary bilateral osteoarthritis of hip
M16.1: Other primary osteoarthritis of hip
M16.9: Osteoarthritis of hip, unspecified
M17 – Osteoarthritis of the Knee
M17.0: Primary bilateral osteoarthritis of knee
M17.1: Other primary osteoarthritis of knee
M17.9: Osteoarthritis of knee, unspecified
M18 – Osteoarthritis of the First Carpometacarpal Joint (Base of Thumb)
M18.0: Primary osteoarthritis, bilateral
M18.9: Osteoarthritis, unspecified
M19 – Other and Unspecified Osteoarthritis
M19.0: Primary osteoarthritis of other joints
M19.9: Osteoarthritis, unspecified site
Why ICD-10 Codes for Osteoarthritis Matter
Accurate ICD-10 coding has several important benefits:
Insurance and Billing – Ensures providers receive proper reimbursement.
Clinical Records – Helps track disease progression and treatment history.
Research and Data Collection – Provides statistics on the prevalence and impact of osteoarthritis.
Public Health Planning – Assists governments and health organizations in understanding the burden of arthritis on healthcare systems.
Diagnosis of Osteoarthritis
To assign the correct ICD-10 code, diagnosis of osteoarthritis is typically confirmed through:
Medical history and symptom review – Pain, stiffness, and functional limitations.
Physical examination – Detecting joint tenderness, swelling, or deformity.
Imaging tests – X-rays reveal joint space narrowing, bone spurs, and cartilage loss.
Lab tests – To rule out other conditions like rheumatoid arthritis.
Management and Treatment of Osteoarthritis
Although there is no cure for osteoarthritis, treatments aim to relieve symptoms, improve mobility, and slow progression.
1. Lifestyle Changes
Weight reduction to relieve joint stress.
Regular low-impact exercise (walking, cycling, swimming).
Joint protection techniques to prevent further damage.
2. Medications
Over-the-counter pain relievers (acetaminophen).
Nonsteroidal anti-inflammatory drugs (NSAIDs).
Corticosteroid injections for severe pain.
3. Physical Therapy
Muscle strengthening exercises.
Stretching and range-of-motion programs.
Assistive devices (braces, orthotics, or canes).
4. Surgical Interventions
Arthroscopy to clean joint surfaces.
Osteotomy to realign bones.
Joint replacement surgery for severe hip or knee osteoarthritis.
Osteoarthritis vs. Other Forms of Arthritis
Osteoarthritis should not be confused with other types of arthritis:
Rheumatoid Arthritis (RA): An autoimmune disorder causing joint inflammation.
Gout: Caused by uric acid crystal deposits in joints.
Psoriatic Arthritis: Linked to psoriasis and immune dysfunction.
ICD-10 codes differentiate these conditions to ensure patients receive correct treatment and accurate billing.
Preventing Osteoarthritis
While osteoarthritis cannot always be prevented, adopting healthy lifestyle habits reduces the risk:
Maintain a healthy body weight.
Engage in regular, low-impact physical activity.
Avoid repetitive stress on joints.
Protect joints from injury with proper techniques.
Eat a nutrient-rich diet to support bone and cartilage health.
Conclusion
Osteoarthritis ICD 10 is a chronic, progressive disease that significantly impacts quality of life. Accurate classification using ICD-10 codes (M15–M19) allows healthcare providers to document and manage the condition effectively, ensuring appropriate treatment, billing, and research opportunities.
By understanding symptoms, risk factors, and coding practices, healthcare professionals can provide better care, while patients can make informed decisions about managing their condition. With lifestyle changes, medical treatments, and accurate documentation, osteoarthritis can be controlled to improve daily function and overall well-being.